Good Health Starts Here.
All Of Your Patient Care Needs
Award-Winning Care





UConn Health has garnered many awards and accolades over the years, and the list continues to grow. We have been recognized for top-quality patient care and groundbreaking research and have been named in the top 10% of hospitals nationally for patient safety.
We’re Seeing Stars
Want to know how patients feel about the care they receive here? Look for the stars. UConn Health uses the Star Rating system to help patients make informed decisions about their care. The ratings are based on our patient experience surveys and are collected by a third-party vendor.
Access Your Records Anywhere, Any Time With MyChart
View Health Records
Access your test results and visit notes from the comfort of your own home.
Manage Your Care
Request an appointment, communicate with your doctor, or request prescription refills.
Proof of COVID-19 Vaccine Status
View your vaccination status with a QR code or a printable PDF.
Pay Your Bill Online
See your account statements and make a payment online.
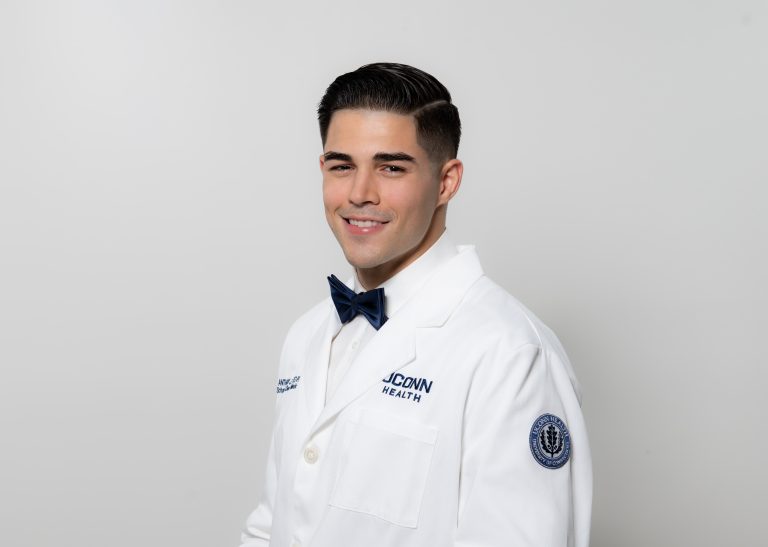
Growing Connecticut’s Health Care Workforce
UConn is Connecticut’s largest single source of new physicians, surgeons, and dentists. 70% of our medical school graduates are Connecticut physicians or resident physicians, and more than 50% of the state's dentists are UConn alumni.